Audit
Basically, there are only two ways for any company to improve its bottom line—increase revenue or decrease costs. Medical billing is a complex process and when the billing covers more complex matters or multiple events, the opportunities for errors multiply and so do the costs. The skill set and experience required to identify and challenge errors is a specialized expertise.
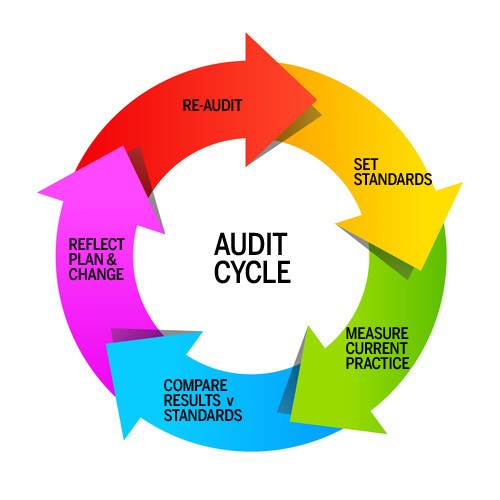
Our Audit procedure is very fair, transparent and we support our claim with evidence thus enabling you to cross match it with your records. Once we compile the results of Audit then we can define a strategy as how to fix these issues and increase your reimbursements/bottom line which is the essence of the audit.
We cover the following areas in Audit :
- Fee Schedule: Are you getting paid by insurance companies what you actually deserve as per your fee schedule and are you billing them the right amount?
- Billing and Coding Discrepancies: Is your billing company doing an outstanding job. Are they familiar with the coding changes and regulations, denied claims % etc.
- Financial Bleeding: How much money have you lost and losing because of billing errors on a monthly basis
- Accounts Receivable: How much is your AR for a particular month that we will do Audit for and also your average time frame to get the payments (Turn Around Time)
- Identification of Weak Areas: Any errors, weak links, improvement areas
- Compiling Audit Results: A detailed Audit report with evidences and numbers in black and white
- Strategy Moving Forward: Suggest the moving forward strategy and how to overcome these areas
By making an audit a part of standard business practice, healthcare providers can add six- or seven-figure savings in their costs back to their bottom line.